© Scott Olson/Getty Images
(Ho hum, not again)
A number of people have written to me pointing out an outbreak of mass hysteria in the UK press about statins protecting against cancer. I suspect this hysteria has been repeated around the world. Here are the headlines from the eponymous
Statins slash risk of death by cancer: They slow tumour growth
by up to 50% reveal major studies
Experts say there is 'overwhelming' evidence that statins can treat cancer
Study showed they cut death rates for bone cancer patients by 55 per cent
GPs should make patients aware of pills' new benefits, researchers say
I have been aware of claims that statins protect against cancer for many years. They pop up on a pretty regular basis. I have tended to ignore them on the basis that, anyone who is stupid enough to believe such research, deserves all the statins they can get.
However, such is the overblown hype this time, that I feel the need to rouse myself from my slumber, and explain why this is just complete rubbish. I don't need to read the original studies to do this. I have read enough of these over the years. I hope this does not sound too arrogant, but I will happily apologise if any single thing I write here proves to be wrong.
Not randomised controlled studies
The studies quoted will not have been randomised and controlled. By which I mean they did not take, say, forty thousand people and split them into two, randomised, groups. One group to take statins the other to take a placebo. Then wait, say, five years to see what difference there was.
These studies will have been observational. By which I mean you look at people taking statins and see what happens to them vs. people who do not take statins. Such studies can show associations between two variables. But they prove causality. (They cannot provide 'overwhelming' evidence of anything either). This is basic science, page one, paragraph one.
Just to provide one example of this. In 1987 a major observational study showed that women taking HRT had a more than forty per cent reduction in heart disease. At which point it was recommended that women took HRT to protect themselves against heart disease. This was, in fact, written into the guidelines of the American College of Physicians. To fail to prescribe HRT was considered medical malpractice in the USA.1
Some years later came the Women's Health Initiative (WHI) study. The first randomised primary prevention trial to use HRT, and 17,000 women were involved.
'Analysis of hazard ratios showed that after 5.2 years, there was a 29% increase in coronary heart disease risk, including an 18% risk of coronary heart disease mortality and a 32% increase risk of nonfatal myocardial infarction. There was a 20% increase in risk of fatal stroke and 50% increase in the risk of non fatal stroke in women assigned to HRT.' 2
So, a 42% reduction in heart disease turned into a 18% risk of dying of heart disease. In short, observational studies are hopelessly unreliable and often turn out to be complete nonsense. And there is a specific reason why I know these statins studies will be complete rubbish, which I will get to.
Relative not absolute risk
Once again, in these studies, we run into the distorting use of relative, not absolute risk. A fifty per cent reduction in risk can mean something, or nothing very much. It depends what the underlying risk was in the first place. In my book I covered the use/misuse of relative risk in some depth.
Let us just say that if your underling risk of dying in the next five years is 50%, reducing that risk by 50% is a big deal. If the risk of dying in the next five years is 0.1%, then reducing that risk by 50% is five hundred times less of a big deal.
As for slowing tumour growth by 50%. Well, that could mean almost anything. Did you reduce tumour growth by 1%, 50% or some other number. And does reducing tumour growth actually reduce the risk of dying? Of course, you will always find some super rare cancer e.g. bone cancer, where death rates are cut by 55%.
I would imagine this meant about three deaths verses seven in bone cancer. Basically, however small the absolute figures can be to get to a relative risk reduction of 55%. I would guess there will be no statistical significance figure attached to this reduction. Many questions, almost none of them well be answered, you will find.
The elephant in the room (raised cholesterol protects against cancer)
Here, however, is the big issue. People with higher cholesterol levels are far less likely to die of cancer. Add this to the fact that people with higher cholesterol levels are far more likely be prescribed statins, and you start off with the most gigantic built in bias that it is possible to find.
In 1992 (before statins were being prescribed to more than a select few) a conference was held to look at low blood cholesterol and associations with mortality3. Going back this far in time is important. After this, statin prescribing makes it very difficult to disentangle those with naturally low, or high, cholesterol levels vs. those who were taking statins.
All the major studies of the time were reviewed, with nearly one million participants. As you can see from my little graph, reproduced from the figures in the paper, as cholesterol levels rise, the risk of cancer falls. For women, if your cholesterol level is below four, the risk of dying of cancer is 38% higher than if your cholesterol level is above 6.2mmol/l. In men we are looking at a 27% greater risk with low cholesterol levels. {See chart)
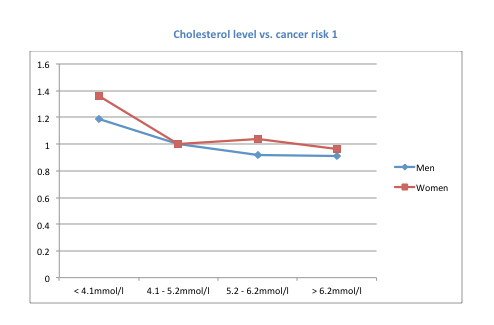
© drmalcolmkendrick.org
Thus any observational study on lowering cholesterol with statins starts off with a massive inbuilt bias in the two populations. You are looking at one group of people who have a much lower risk of cancer to start with, then giving them statins, then declaring that statins protect against cancer..... just most absolute unscientific codswallop.
As final warning. Be careful about lowering cholesterol too far. A very large Japanese study (that you will never have heard of, because it was not very supportive of statins) looked at prescribing statins to over forty seven thousand people over six years. As they found:
'The patients with an exceptionally low TC (total cholesterol) concentration, the so-called 'hyper-responders' to simvastatin, had a higher relative risk of death from malignancy than in the other patient groups.'4
In fact, the rate of death from cancer in those whose cholesterol fell the most dramatically was increased by three hundred and thirty per cent (relative risk, apologies for doing this, but I do not know the absolute risk). The authors added this warning:
'Further analysis is necessary to elucidate why the hyper-responders had an increased risk of death; their baseline characteristics will be described and discussed in detail in the future. Nevertheless, the health of patients who show a remarkable decrease in TC or LDL-C concentration with low-dose statin therapy should be monitored closely.'
Can I return to my slumbers on this issue now?
References
1: American College of Phyisicians. Guidelines for Counselling Post-Menopausal Women about Preventative Hormone Therapy. 117:1038-41. (1992)
2: Writing group for the Women's Health Initiative Investigators. 'Risks and benefits of oestrogen plus progestin in healthy postmenopausal women. Principal results from the Women's Health Initiative Randomized controlled Trials' (2002)
3: Jabobs et al: Conference on Low Blood Cholesterol and Mortality: Vol 86, No 3 September 1992
4: Matsuzaki M et al: Large Scale Cohort Study of the Relationship Between Serum Cholesterol Concentration and Coronary Events With Low-Dose Simvastatin Therapy in Japanese Patients With Hypercholesterolemia Primary Prevention Cohort Study of the Japan Lipid Intervention Trial (J-LIT). 2002; 66: 1087 - 1095




